CellEct Bio (Stem Cell Therapy), by Dan Ganz
Background on CellEct Biotechnology
Overview
CellEct is a company that seeks to overcome the issues of Bone Marrow Transplant (BMT) through hematopoietic stem cell (HSC) therapy. In addition, they are seeking to use the apoptosis-agent resistant characteristic of HSC to differentiate them from other cells in a given sample from blood or bone marrow. Today, HSC therapy is very underdeveloped and only used on deathly ill patients.
HSC are multipotent stem cells, meaning they are undifferentiated cells that can turn into a limited number of tissue or cell types. See below for further HSC background. HSC can be derived from bone marrow, umbilical cord blood, and from blood itself. However, they are most common in bone marrow. BMT can be a very difficult and painful procedure with lots of potential side effects such as Graft versus Host disease, or GvHD. GvHD results from a rejection of the host from donor stem cells. One of the goals of CellEct is to eliminate all side effects of BMT.[1]
Bone Marrow Transplants
Bone Marrow Transplant (BMT) is often offered to those who have defect in their blood cells. Such defects include but are not limited to sickle cell anemia, aplastic anemia, and leukemia. It is the most common stem cell therapy in modern day medicine.[2] Three different types of BMT are considered when a patient is in need. Autologous BMT is when the patient's own stem cells are removed from the marrow then subsequently treated with chemotherapy to kill diseased cells. Allogeneic BMT is when stem cells are taken from a stem cell 'donor'. This donor must be match the genetic makeup as the host in order to avoid rejection. Rejection can result, as discussed above, in GvHD. A match can be detected by a variety of blood tests. These two transplants are often painful due to the injection of a needle into the bone for removal of bone marrow.
Finally, HSC can be taken from umbilical cord blood. Once a baby is born, HSC can be removed from the umbilical cord and then used for transplant. Due to immaturity of umbilical-derived HSC, they are more likely to match the host than an adult bone-marrow donor. Once chemotherapy is performed on the patient/host, HSC can be injected via a central venous catheter.[3]
Diseases Treated with Bone Marrow Transplant
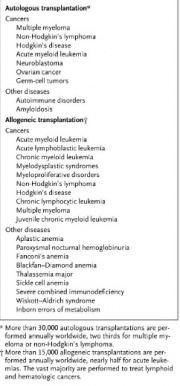
Table 1 lists diseases commonly treated with BMT. As described, most blood disorders are treated with BMT.
Company Goal
Because HSC are very hard to isolate, Cellect is seeking to use unique characteristics to separate HSC from other cells in order to eliminate probability of rejection by host. This includes elimination of GvHD. HSC resistance to apoptosis-inducing agents is the characteristic Cellect is looking to take advantage of. This is all to produce a viable alternative to BMT.
Hematopoietic Stem Cells
Hematopoietic Stem Cells (HSC) are multipotent stem cells that can differentiate into blood and immune system cells. These cells include lymphocytes, macrophages, monocytes, erythrocytes, neutrophil and platelets. The human body uses HSC to regenerate these cell types on its own. Every 1 in approximately 10,000 bone marrow cells are HSC, and every 1 in 100,000 blood cells are HSC.[1] HSC are tough to identify due to their identical behavior to white blood cells in culture.[4] In order to identify HSC in a sample of blood or bone marrow cells, one can test the presence of various surface markers such as CD34, CD38, and CD133. See Table 2 for a list of markers that can be used to identify HSC.

Hematopoietic Stem Cell Transplant History
HSC Transplants began in the early 1970s. The CIty of Hope Cancer Center is a leader in HSC transplantation. As of today, they have performed 10,600 BST transplants. Treatments include patients with leukemias, lymphomas, Hodgkin's disease, myelodyplastic syndromes, and myeloproliferative disorders. [6]
Although HSC are difficult to identify and isolate due to their low populations, a very small is needed for therapy. In fact, less than 100 cells are enough for transplantation. HSC grow extremely quickly and thus an extremely small amount can be used to treat patients.
According to the world marrow donor association, in 2006, about 50,000 HSC transplants took place. 57% of those were autologuos, and 43% were allogeneic. Of the allogenic transplants, 55% were from family donors and 45% from unrelated donors. Of those were got HSC transplants, 54.5% has lymphoproliferative disorders, and 33.8% had leukemias.[7]
CellEct findings
CellEct also shared preclinical data on their site. In their study, they used HSC from all sources (bone marrow, umbilical chord, and blood). They also used HSC from close relatives and completely unrelated subjects in both human and murine experiments.[1] Major findings include:
-Resistance to receptor-mediated apoptosis is common in HSC. This is achieved by up-regulation of anti-apoptotic mechanisms at the transcription level
-As HSC begin to differentiate, they begin to respond to receptor-mediated apoptotic signals
-HSC resistant to receptor-mediated apoptosis are used for engraftment
Indications
Today, HSC transplantation remains highly risky and is only advised for patients that are deathly ill. The high risk is mainly due to immunity; HSC transplants are still a new idea and thus further research is required to reduce immune system rejection. Those patients who receive HSC transplants do not benefit from chemotherapeutic treatment. Candidates include:
-Minors with inborn defects such as congenital neutropenia, severe combined immunodeficiency, aplastic anemia[8]
-Adults with aplastic anemia who lack stem cells
-Individuals with sickle-cell disease, myelodysplastic syndrome, neuroblastoma, lymphoma, Ewing's Sarcoma, Desmoplastic small round cell tumor, chronic granulomatous disease and Hodgkin's disease.[9]
-Elders can also receive HST transplants in small doses.
References
[1]."Cellect Bio." Cellect Bio. Web. 19 Feb. 2012. <http://www.cellectbio.com/>
[2]. "Human Stem Cells at Johns Hopkins: A Forty Year History." Stem Cell Research at Johns Hopkins Medicine: History of Bone Marrow Transplants. Web. 20 Feb. 2012. <http://www.hopkinsmedicine.org/stem_cell_research/cell_therapy/human_stem_cells_johns_hopkins.html>.
[3]."Bone Marrow Transplant." U.S National Library of Medicine. U.S. National Library of Medicine. Web. 20 Feb. 2012. <http://www.nlm.nih.gov/medlineplus/ency/article/003009.htm>.
[4]. "Hematopoietic Stem Cells." National Institute of Health. Web. 20 Feb. 2012. <http://stemcells.nih.gov/info/scireport/chapter5.asp>
[5]. Copelan, E. A. "Hematopoietic stem-cell transplantation". The New England Journal of Medicine. 2006
[6]. "City of Hope." Cityofhope.org. Web. 22 Feb. 2012. <http://www.cityofhope.org/patient_care/treatments/HCT/Pages/default.aspx>.
[7]. "Worldwide Marrow Donor Association." WMDA. Web. 21 Feb. 2012. <http://www.worldmarrow.org/>.
[8]. "Supplemental Content." National Center for Biotechnology Information. U.S. National Library of Medicine. Web. 22 Feb. 2012. <http://www.ncbi.nlm.nih.gov/pubmed/17229630>.
[9]. "Current Uses and Outcomes of Hematopoietic Stem Cell Transplantation 2009." MCW. MCW.edu. Web. 21 Feb. 2012. <https://campus.mcw.edu/AngelUploads/Content/CS_IBMTR2/_assoc/ECCBED0AF0A4492BB667FB6227DC7C06/summary05_Pt1_files/frame.htm>.
