Klinke:Research: Difference between revisions
No edit summary |
|||
| (11 intermediate revisions by the same user not shown) | |||
| Line 3: | Line 3: | ||
=== Summary of Research Program === | === Summary of Research Program === | ||
''' | ''' | ||
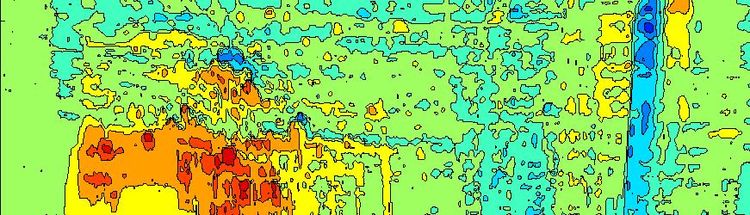
[[Image:Klinke-ResearchSummary.jpg| | [[Image:Klinke-ResearchSummary.jpg|350px|left|Schematic diagram of research program.]] | ||
While intriguing cancer immunologists as a target for over a century, evading immune destruction has only recently been identified as an emerging hallmark of cancer. Our progress towards realizing cancer immunotherapy is limited by our understanding of the biology and the predominant mode of scientific inquiry. Specifically, one of the major barriers to progress is that pre-clinical development of molecular targeted therapies primarily focus on the response of the cancer cell alone to novel targets. This approach assumes that the therapeutic response to tumors can be defined based upon simple input (i.e., drug dosage) simple output (i.e., tumor regression) relationships. Emerging evidence paints a more complicated picture that tumor response to therapy reflects a prolonged dialogue between malignant, stromal, and immune cells of the host. This evidence implies that cancer is an integrated closed-loop system: a multi-component system where the output (e.g., cell response) of one component provides the input (e.g., a biochemical cue) to another component. The response of a patient to therapy is therefore influenced by overall system input and by crosstalk among neighboring cells that we are just beginning to unravel. To improve our understanding of the biology, we have focused on three aspects of this problem, as summarized in the graphic. The first research direction focuses on identifying the internal circuitry that governs how malignant cells interpret environmental signals and how this internal circuitry becomes re-wired during oncogenesis (i.e., How do malignant cells interpret these biochemical signals?). This internal circuitry governs how a cell processes information and makes decisions (i.e., whether it proliferates, doesn't do anything, or dies). The second research direction focuses on identifying the rules that govern how immune cells interpret environmental signals and how to parse intracellular signaling events from population-level phenomena (i.e., How do immune cells interpret these biochemical signals?). The third research direction focuses on identifying the biochemical cues, as either secreted proteins or coding and non-coding RNA contained within exosomes, that cells use to shape their local environment (i.e., What biochemical signals do cells use to communicate?). A Bayesian perspective permeates throughout the work - designing experiments that minimize the influence of a priori bias (e.g., proteomics and high content assays) and analyzing data in a way that maximizes insight into system behavior (e.g., model-based inference). | |||
Model-based inference is the process of encoding our prior knowledge of how cells interpret biochemical signals in the form of a mathematical model. The model is then used to test whether our prior knowledge is consistent with the experimental data. Model-based inference is a key tool as biological systems exhibit intrinsic uncertainty - due to either ethical constraints or due to technical limitations of the available experimental techniques. By combining experimental study with model-based inference, we hope to obtain greater fidelity in understanding how these systems work than could be obtained using either technique in isolation. | |||
''' | ''' | ||
=== Integrative Systems Approach to Identify Local Oncogenic Modulation of the IL12 Axis === | |||
'''Collaborators: J. Michael Ruppert, Yon Rojanasakul, West Virginia University''' <br> | |||
'''Funding source: National Cancer Institute''' <br> | |||
Immunotherapies, like immune checkpoint modulators, are poised to transform the therapeutic landscape for cancer. While these therapies elicit remarkable responses in a subset of patients, a key hurdle for broadening the clinical benefit is identifying collateral targets that relieve tumor-induced changes in the tissue microenvironment that block endogenous anti-tumor signals. To identify these collateral targets, we have developed a phenotypic screen to identify mechanisms that malignant cells use to block immune cell response to cytokines that promote anti-tumor immunity, such as Interleukin-12. The objective of this Bioengineering Research Grant is to identify collateral targets in breast and lung carcinomas by screening a set of transplantable models for these cancers and to validate these targets using pre-clinical mouse models and human data. Given that oncogenesis is an evolutionary process involving repeated mutation and selection, our central hypothesis is that malignant cells evolve to secrete proteins that collectively cross-regulate the response of CD4+ and CD8+ T cells to Interleukin-12 (IL12), a potent adjuvant of anti-tumor immunity. To test our central hypothesis, we will first establish conditions where a T cell response to IL12 can be predicted using a mechanistic math model. Next, we will recreate tumor-induced immunosuppression in vitro, where the mathematical model will be used to define how the T cell response to IL12 is altered upon co-culture with the different transplantable models for lung and breast cancer. Proteins secreted by tumor cells that recreate the observed phenotype will be identified using LC-MS/MS-based proteomics. Immunosuppressive mechanisms identified in vitro will be validated using pre-clinical mouse models and a retrospective cohort study using data obtained from large cancer studies that relate `omics with clinical outcomes. This multidisciplinary approach is projected to yield the following expected outcomes: 1) enable stratifying patients based on mechanistic pathology, 2) guide developing drugs against these collateral targets, and 3) identify patient cohorts that are likely to benefit from specific combination immunotherapies. | |||
=== Cell Heterogeneity and Emergent Trastuzumab Resistance in Breast Cancer === | === Cell Heterogeneity and Emergent Trastuzumab Resistance in Breast Cancer === | ||
''' | '''Collaborators: J. Michael Ruppert, West Virginia University''' <br> | ||
'''Funding source: PhRMA Foundation, National Cancer Institute''' <br> | '''Funding source: PhRMA Foundation, National Cancer Institute''' <br> | ||
| Line 18: | Line 24: | ||
''' | ''' | ||
=== CAREER: Interrogating Antagonistic Mechanisms of Signaling Cross-talk in Natural Killer Cells === | === CAREER: Interrogating Antagonistic Mechanisms of Signaling Cross-talk in Natural Killer Cells === | ||
'''Collaborators: Jonathan Bramson, McMaster University, Hamilton, ON''' <br> | '''Collaborators: Jonathan Bramson, McMaster University, Hamilton, ON''' <br> | ||
'''Funding source: National Science Foundation''' <br> | '''Funding source: National Science Foundation''' <br> | ||
[[Image:SEM-B16F0-Exosome.TIF|thumb|right|A scanning electron micrograph of exosomes - nanoscale structures - obtained from a melanoma cancer cell line that are thought to play a role in cell-to-cell communication.]] | |||
This NSF award by the Biotechnology, Biochemical and Biomass Engineering program supports work to improve our fundamental understanding of how cancer cells escape the cytotoxic action of monoclonal antibodies. Monoclonal antibodies comprise one of the largest classes of cancer drugs that target molecules unique to cancer cells. However, the emergence of resistance to molecular targeted therapies is an increasing, and poorly understood, problem. Without improved understanding of how cancer cells resist the action of molecular targeted therapies, designing effective treatments will remain limited. To improve ultimately the effectiveness of mAbs as cancer drugs, we propose a conceptually novel approach that combines aspects of cellular engineering, immunology, cancer biology, and computationally intensive model-based inference. The research objectives are integrated with educational objectives that aim to promote cross-disciplinary communication among experts and to improve the ability of scientists and engineers to communicate scientific concepts, like how theory and computation are used in scientific practice, effectively with the lay public. It is expected that these aims will have an impact that ranges from local to international. At the local level, the proposed research will provide interdisciplinary training opportunities for graduate and undergraduate students at the interface between multiple disciplines, including biochemical engineering, cancer biology, molecular biology, immunology, and pharmacology. The proposed education aims will also focus outward to create scientists and engineers that can collaborate more effectively across disciplines and, more importantly, that can convey what they do and it's importance to the lay public. Finally, the fundamental fruits of this research may be applied to improve therapies for cancer, a disease that, in developed countries, kills one in three. | This NSF award by the Biotechnology, Biochemical and Biomass Engineering program supports work to improve our fundamental understanding of how cancer cells escape the cytotoxic action of monoclonal antibodies. Monoclonal antibodies comprise one of the largest classes of cancer drugs that target molecules unique to cancer cells. However, the emergence of resistance to molecular targeted therapies is an increasing, and poorly understood, problem. Without improved understanding of how cancer cells resist the action of molecular targeted therapies, designing effective treatments will remain limited. To improve ultimately the effectiveness of mAbs as cancer drugs, we propose a conceptually novel approach that combines aspects of cellular engineering, immunology, cancer biology, and computationally intensive model-based inference. The research objectives are integrated with educational objectives that aim to promote cross-disciplinary communication among experts and to improve the ability of scientists and engineers to communicate scientific concepts, like how theory and computation are used in scientific practice, effectively with the lay public. It is expected that these aims will have an impact that ranges from local to international. At the local level, the proposed research will provide interdisciplinary training opportunities for graduate and undergraduate students at the interface between multiple disciplines, including biochemical engineering, cancer biology, molecular biology, immunology, and pharmacology. The proposed education aims will also focus outward to create scientists and engineers that can collaborate more effectively across disciplines and, more importantly, that can convey what they do and it's importance to the lay public. Finally, the fundamental fruits of this research may be applied to improve therapies for cancer, a disease that, in developed countries, kills one in three. | ||
''' | ''' | ||
<!-- | |||
<script> | |||
(function(i,s,o,g,r,a,m){i['GoogleAnalyticsObject']=r;i[r]=i[r]||function(){ | |||
(i[r].q=i[r].q||[]).push(arguments)},i[r].l=1*new Date();a=s.createElement(o), | |||
m=s.getElementsByTagName(o)[0];a.async=1;a.src=g;m.parentNode.insertBefore(a,m) | |||
})(window,document,'script','//www.google-analytics.com/analytics.js','ga'); | |||
ga('create', 'UA-53312470-1', 'auto'); | |||
ga('send', 'pageview'); | |||
</script> | |||
--> | |||
Revision as of 09:25, 18 April 2016
The Klinke Lab @ West Virginia University
Home
Research
Lab Members
Publications
Talks
Positions
Contact
Summary of Research Program

While intriguing cancer immunologists as a target for over a century, evading immune destruction has only recently been identified as an emerging hallmark of cancer. Our progress towards realizing cancer immunotherapy is limited by our understanding of the biology and the predominant mode of scientific inquiry. Specifically, one of the major barriers to progress is that pre-clinical development of molecular targeted therapies primarily focus on the response of the cancer cell alone to novel targets. This approach assumes that the therapeutic response to tumors can be defined based upon simple input (i.e., drug dosage) simple output (i.e., tumor regression) relationships. Emerging evidence paints a more complicated picture that tumor response to therapy reflects a prolonged dialogue between malignant, stromal, and immune cells of the host. This evidence implies that cancer is an integrated closed-loop system: a multi-component system where the output (e.g., cell response) of one component provides the input (e.g., a biochemical cue) to another component. The response of a patient to therapy is therefore influenced by overall system input and by crosstalk among neighboring cells that we are just beginning to unravel. To improve our understanding of the biology, we have focused on three aspects of this problem, as summarized in the graphic. The first research direction focuses on identifying the internal circuitry that governs how malignant cells interpret environmental signals and how this internal circuitry becomes re-wired during oncogenesis (i.e., How do malignant cells interpret these biochemical signals?). This internal circuitry governs how a cell processes information and makes decisions (i.e., whether it proliferates, doesn't do anything, or dies). The second research direction focuses on identifying the rules that govern how immune cells interpret environmental signals and how to parse intracellular signaling events from population-level phenomena (i.e., How do immune cells interpret these biochemical signals?). The third research direction focuses on identifying the biochemical cues, as either secreted proteins or coding and non-coding RNA contained within exosomes, that cells use to shape their local environment (i.e., What biochemical signals do cells use to communicate?). A Bayesian perspective permeates throughout the work - designing experiments that minimize the influence of a priori bias (e.g., proteomics and high content assays) and analyzing data in a way that maximizes insight into system behavior (e.g., model-based inference).
Model-based inference is the process of encoding our prior knowledge of how cells interpret biochemical signals in the form of a mathematical model. The model is then used to test whether our prior knowledge is consistent with the experimental data. Model-based inference is a key tool as biological systems exhibit intrinsic uncertainty - due to either ethical constraints or due to technical limitations of the available experimental techniques. By combining experimental study with model-based inference, we hope to obtain greater fidelity in understanding how these systems work than could be obtained using either technique in isolation.
Integrative Systems Approach to Identify Local Oncogenic Modulation of the IL12 Axis
Collaborators: J. Michael Ruppert, Yon Rojanasakul, West Virginia University
Funding source: National Cancer Institute
Immunotherapies, like immune checkpoint modulators, are poised to transform the therapeutic landscape for cancer. While these therapies elicit remarkable responses in a subset of patients, a key hurdle for broadening the clinical benefit is identifying collateral targets that relieve tumor-induced changes in the tissue microenvironment that block endogenous anti-tumor signals. To identify these collateral targets, we have developed a phenotypic screen to identify mechanisms that malignant cells use to block immune cell response to cytokines that promote anti-tumor immunity, such as Interleukin-12. The objective of this Bioengineering Research Grant is to identify collateral targets in breast and lung carcinomas by screening a set of transplantable models for these cancers and to validate these targets using pre-clinical mouse models and human data. Given that oncogenesis is an evolutionary process involving repeated mutation and selection, our central hypothesis is that malignant cells evolve to secrete proteins that collectively cross-regulate the response of CD4+ and CD8+ T cells to Interleukin-12 (IL12), a potent adjuvant of anti-tumor immunity. To test our central hypothesis, we will first establish conditions where a T cell response to IL12 can be predicted using a mechanistic math model. Next, we will recreate tumor-induced immunosuppression in vitro, where the mathematical model will be used to define how the T cell response to IL12 is altered upon co-culture with the different transplantable models for lung and breast cancer. Proteins secreted by tumor cells that recreate the observed phenotype will be identified using LC-MS/MS-based proteomics. Immunosuppressive mechanisms identified in vitro will be validated using pre-clinical mouse models and a retrospective cohort study using data obtained from large cancer studies that relate `omics with clinical outcomes. This multidisciplinary approach is projected to yield the following expected outcomes: 1) enable stratifying patients based on mechanistic pathology, 2) guide developing drugs against these collateral targets, and 3) identify patient cohorts that are likely to benefit from specific combination immunotherapies.
Cell Heterogeneity and Emergent Trastuzumab Resistance in Breast Cancer
Collaborators: J. Michael Ruppert, West Virginia University
Funding source: PhRMA Foundation, National Cancer Institute

Monoclonal antibodies, such as trastuzumab, are one of the largest categories of new drugs that target specifically molecules that differentiate cancer cells from normal cells. Despite the remarkable clinical efficacy and specificity of these molecularly targeted therapies, acquired and de novo resistance to therapy is an important clinical problem. Understanding emergent resistance to trastuzumab is inhibited by the inability to quantify aberrant cell signaling pathways among heterogeneous populations of breast cancer cells. Thus there is urgent need for multidisciplinary approaches to assess and interpret the clinical importance of cellular heterogeneity within breast cancer tumors. Our long-term goal is to improve the clinical management of cancer by establishing the scientific foundation for a prognostic technology that will identify individuals who will develop resistance to molecularly targeted therapies. The overall objective of this project is to identify unique patterns of signaling proteins associated with drug sensitivity and apply computational tools from chemical kinetics and Bayesian statistics to interpret the significance of these patterns of protein expression. Our central hypothesis is that breast cancer cells that overexpress ErbB2 exhibit heterogeneity in response to trastuzumab. Furthermore, this heterogeneity is due to variations in expression of proteins that influence the ErbB2 signaling pathway. Prior studies identify such proteins that individually correlate with trastuzumab resistance. The challenge is inferring how these proteins act in concert to influence trastuzumab resistance. The rationale that underlies the proposed research is that identifying patterns of signaling proteins that are correlated with sensitivity to trastuzumab will enable measuring these protein patterns at the single-cell level in tumor biopsy samples. The proposed research is innovative as it provides a novel approach that combines cutting-edge techniques in computational systems biology and proteomics to address the pressing issue of emergent resistance to trastuzumab in breast cancer patients.
CAREER: Interrogating Antagonistic Mechanisms of Signaling Cross-talk in Natural Killer Cells
Collaborators: Jonathan Bramson, McMaster University, Hamilton, ON
Funding source: National Science Foundation

This NSF award by the Biotechnology, Biochemical and Biomass Engineering program supports work to improve our fundamental understanding of how cancer cells escape the cytotoxic action of monoclonal antibodies. Monoclonal antibodies comprise one of the largest classes of cancer drugs that target molecules unique to cancer cells. However, the emergence of resistance to molecular targeted therapies is an increasing, and poorly understood, problem. Without improved understanding of how cancer cells resist the action of molecular targeted therapies, designing effective treatments will remain limited. To improve ultimately the effectiveness of mAbs as cancer drugs, we propose a conceptually novel approach that combines aspects of cellular engineering, immunology, cancer biology, and computationally intensive model-based inference. The research objectives are integrated with educational objectives that aim to promote cross-disciplinary communication among experts and to improve the ability of scientists and engineers to communicate scientific concepts, like how theory and computation are used in scientific practice, effectively with the lay public. It is expected that these aims will have an impact that ranges from local to international. At the local level, the proposed research will provide interdisciplinary training opportunities for graduate and undergraduate students at the interface between multiple disciplines, including biochemical engineering, cancer biology, molecular biology, immunology, and pharmacology. The proposed education aims will also focus outward to create scientists and engineers that can collaborate more effectively across disciplines and, more importantly, that can convey what they do and it's importance to the lay public. Finally, the fundamental fruits of this research may be applied to improve therapies for cancer, a disease that, in developed countries, kills one in three.