Yeo lab:Projects: Difference between revisions
No edit summary |
|||
| Line 6: | Line 6: | ||
We strive to make a significant impact in public health through research. The goal of our research is to develop new drug delivery systems and biomaterials, which will enable a safe, efficient, and clinically viable delivery of drugs, genes, and/or cells in a target-specific manner. | We strive to make a significant impact in public health through research. The goal of our research is to develop new drug delivery systems and biomaterials, which will enable a safe, efficient, and clinically viable delivery of drugs, genes, and/or cells in a target-specific manner. | ||
== Tumor | == Tumor-targeted drug delivery == | ||
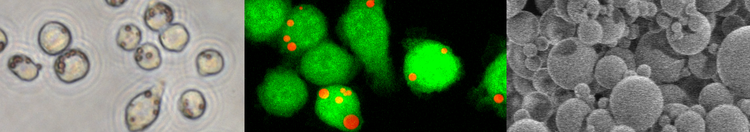
In developing safe and effective chemotherapy, it is | In developing safe and effective chemotherapy, it is crucial to engineer a targeted drug delivery system that can selectively deliver antiproliferative drugs to tumor cells without affecting normal cells. While extensive efforts are being made to enhance the recognition of drug carriers by tumor tissues, the targeting effect mostly depends on the imperfect vasculature of tumors, which leads to preferential extravasation of drug carriers, and the contribution of targeting ligands is rather minimal. This limitation in current targeting strategy is due in part to the diversity and heterogeneity of the tumor cells and may also be related to the fact that the endothelium surrounding tumors (peritumoral endothelium) limits direct access of drug carriers to the underlying tissues. Another challenge in tumor-targeted drug delivery is that many drug carriers are not stable in the presence of hydrophobic components such as serum proteins or lipids, as we have shown with poly(lactic-co-glycolic acid) (PLGA) nanoparticles (NPs). The instability of drug carriers leads to premature release of the entrapped drugs during circulation. | ||
We try to address these challenges in three ways, which will be combined in future studies. One approach is to develop a nanocarrier system that remains inert without releasing drugs in normal tissues but changes into a cell-interactive form by common features of tumor microenvironment such as pH or overexpressed enzymes. For example, we have developed a new biocompatible chitosan derivative, which shows zwitterionic charge profiles similar to those of proteins. We have proven that the chitosan derivative (zwitterionic chitosan, ZWC) can serve as a conditional stealth coating material for nanocarriers, which prevent random interaction of the carriers with normal tissues or serum proteins but allow high-affinity interactions with cells in the acidic environment of hypoxic tumors. The other approach is to engineer a nanocarrier surface to enhance its extravasation at tumor tissues. To this end, NPs are decorated with a quinic acid derivative, a small molecule mimic of E-selectin that binds to sialyl Lewis-x on the endothelium surrounding tumors. Another approach is to produce drug nanocrystals with high lattice energy, which remain stable in circulation for a prolonged period of time without leaching out free drug until they reach tumors. The nanocrystals are coated with intact albumin to protect them from the reticuloendothelial system and improve their interactions with tumor tissues via albumin-receptor mediated interactions. | |||
Related articles | |||
== Inhalational Drug Delivery for Chronic Pulmonary Diseases == | == Inhalational Drug Delivery for Chronic Pulmonary Diseases == | ||
Revision as of 15:02, 19 August 2017
|
We strive to make a significant impact in public health through research. The goal of our research is to develop new drug delivery systems and biomaterials, which will enable a safe, efficient, and clinically viable delivery of drugs, genes, and/or cells in a target-specific manner. Tumor-targeted drug deliveryIn developing safe and effective chemotherapy, it is crucial to engineer a targeted drug delivery system that can selectively deliver antiproliferative drugs to tumor cells without affecting normal cells. While extensive efforts are being made to enhance the recognition of drug carriers by tumor tissues, the targeting effect mostly depends on the imperfect vasculature of tumors, which leads to preferential extravasation of drug carriers, and the contribution of targeting ligands is rather minimal. This limitation in current targeting strategy is due in part to the diversity and heterogeneity of the tumor cells and may also be related to the fact that the endothelium surrounding tumors (peritumoral endothelium) limits direct access of drug carriers to the underlying tissues. Another challenge in tumor-targeted drug delivery is that many drug carriers are not stable in the presence of hydrophobic components such as serum proteins or lipids, as we have shown with poly(lactic-co-glycolic acid) (PLGA) nanoparticles (NPs). The instability of drug carriers leads to premature release of the entrapped drugs during circulation. We try to address these challenges in three ways, which will be combined in future studies. One approach is to develop a nanocarrier system that remains inert without releasing drugs in normal tissues but changes into a cell-interactive form by common features of tumor microenvironment such as pH or overexpressed enzymes. For example, we have developed a new biocompatible chitosan derivative, which shows zwitterionic charge profiles similar to those of proteins. We have proven that the chitosan derivative (zwitterionic chitosan, ZWC) can serve as a conditional stealth coating material for nanocarriers, which prevent random interaction of the carriers with normal tissues or serum proteins but allow high-affinity interactions with cells in the acidic environment of hypoxic tumors. The other approach is to engineer a nanocarrier surface to enhance its extravasation at tumor tissues. To this end, NPs are decorated with a quinic acid derivative, a small molecule mimic of E-selectin that binds to sialyl Lewis-x on the endothelium surrounding tumors. Another approach is to produce drug nanocrystals with high lattice energy, which remain stable in circulation for a prolonged period of time without leaching out free drug until they reach tumors. The nanocrystals are coated with intact albumin to protect them from the reticuloendothelial system and improve their interactions with tumor tissues via albumin-receptor mediated interactions. Related articles Inhalational Drug Delivery for Chronic Pulmonary DiseasesInhalable microparticles are an attractive treatment option for chronic pulmonary diseases such as cystic fibrosis, asthma, or chronic obstructive pulmonary disease, because they can provide efficient local medication with minimal systemic side effects, a prolonged therapeutic effect, and an easy way of administration. Recent advances in particle technology have overcome a number of hurdles in achieving microparticles with favorable aerodynamic properties. However, existing technologies do not adequately address biological barriers specific to the pulmonary diseases. We recognize that mucus layer on the lung epithelium is a significant barrier for pulmonary drug delivery, especially in therapy of cystic fibrosis and obstructive lung diseases. When this barrier is effectively overcome, inhalational drug delivery systems will open up new opportunities for these devastating diseases. With this challenge in mind, our laboratory has recently produced and evaluated a spray-dried powder containing both DNase and ciprofloxacin. We now have a proof of principle that simultaneous delivery of a drug along with a mucolytic agent can facilitate diffusion of the drug and enhance its efficacy and, consequently, reduce the dose requirement for inhaled powder. Our goal is to extend this principle to develop inhalable gene delivery system consisting of mucolytic sugars and a new gene-polymer complex recently developed in our lab for gene therapy of cystic fibrosis. Biomaterials and Drug Delivery Systems for Functional Repair of Damaged TissuesTwo research endeavors are made in the area of in-situ tissue regeneration. One is to engineer functional cardiac tissues in situ by delivering microencapsulated growth factors and cardiomyocytes using an in-situ crosslinkable hydrogel. The lack of success in cell therapy of myocardial infarction (MI) is attributed to the significant cell loss following transplantation, resulting from limited cell survival and maintenance of surviving cells. We hypothesize that timely supply of essential combinations of growth factors will improve the survival and functional development of implanted cardiomyocytes and increase the success rate of the cell-based MI therapy. The other application is to utilize the in-situ crosslinkable hydrogel for assisting in fusion of severed spinal cords. While no effective therapies to treat nerves that are completely severed currently exist, it is shown that function of transected nerves can be immediately restored ex vivo by application of polyethylene glycol. However, the nerve repair technique has not been successful in vivo. One of the reasons may be that the bond reconnecting nerves is easily damaged by tissue micromotion. We hypothesize that a bioadhesive chitosan hydrogel would stabilize the severed nerves and facilitate functional recovery. |