Yeo lab:Projects: Difference between revisions
| Line 71: | Line 71: | ||
*Bajaj, G., Kim, M.R., Mohammed, S.I., and Yeo, Y.: Hyaluronic acid-based hydrogel for local delivery of paclitaxel in Intraperitoneal tumors. J. Control. Release. [http://dx.doi.org/10.1016/j.jconrel.2011.12.001 (2012) 158(3): 386-392]. | *Bajaj, G., Kim, M.R., Mohammed, S.I., and Yeo, Y.: Hyaluronic acid-based hydrogel for local delivery of paclitaxel in Intraperitoneal tumors. J. Control. Release. [http://dx.doi.org/10.1016/j.jconrel.2011.12.001 (2012) 158(3): 386-392]. | ||
*Bajaj, G. and Yeo, Y.: Drug delivery systems for intraperitoneal therapy. Pharm. Res. (2010) 27(5): [http://dx.doi.org/10.1007/s11095-009-0031-z 735-738]. | *Bajaj, G. and Yeo, Y.: Drug delivery systems for intraperitoneal therapy. Pharm. Res. (2010) 27(5): [http://dx.doi.org/10.1007/s11095-009-0031-z 735-738]. | ||
|}{{Yeo_end_tool}}<br style="clear:both" /> | |}{{Yeo_end_tool}}<br style="clear:both" /> | ||
Revision as of 21:59, 19 August 2017
|
We strive to make a significant impact in public health through research. The goal of our research is to develop new drug delivery systems and biomaterials, which will enable a safe, efficient, and clinically viable delivery of drugs, genes, and/or cells in a target-specific manner.
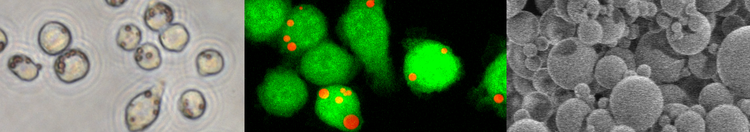
Tumor-targeted drug deliveryIn developing safe and effective chemotherapy, it is crucial to engineer a targeted drug delivery system that can selectively deliver antiproliferative drugs to tumor cells without affecting normal cells. While extensive efforts are being made to enhance the recognition of drug carriers by tumor tissues, the targeting effect mostly depends on the imperfect vasculature of tumors, which leads to preferential extravasation of drug carriers, and the contribution of targeting ligands is rather minimal. This limitation in current targeting strategy is due in part to the diversity and heterogeneity of the tumor cells and may also be related to the fact that the endothelium surrounding tumors (peritumoral endothelium) limits direct access of drug carriers to the underlying tissues. Another challenge in tumor-targeted drug delivery is that many drug carriers are not stable in the presence of hydrophobic components such as serum proteins or lipids, as we have shown with poly(lactic-co-glycolic acid) (PLGA) nanoparticles (NPs). The instability of drug carriers leads to premature release of the entrapped drugs during circulation. We try to address these challenges in three ways, which will be combined in future studies. One approach is to develop a nanocarrier system that remains inert without releasing drugs in normal tissues but changes into a cell-interactive form by common features of tumor microenvironment such as pH or overexpressed enzymes. For example, we have developed a new biocompatible chitosan derivative, which shows zwitterionic charge profiles similar to those of proteins. We have proven that the chitosan derivative (zwitterionic chitosan, ZWC) can serve as a conditional stealth coating material for nanocarriers, which prevent random interaction of the carriers with normal tissues or serum proteins but allow high-affinity interactions with cells in the acidic environment of hypoxic tumors. The other approach is to engineer a nanocarrier surface to enhance its extravasation at tumor tissues. To this end, NPs are decorated with a quinic acid derivative, a small molecule mimic of E-selectin that binds to sialyl Lewis-x on the endothelium surrounding tumors. Another approach is to produce drug nanocrystals with high lattice energy, which remain stable in circulation for a prolonged period of time without leaching out free drug until they reach tumors. The nanocrystals are coated with intact albumin to protect them from the reticuloendothelial system and improve their interactions with tumor tissues via albumin-receptor mediated interactions. Related publications
Nanoparticle surface engineeringIn an effort to facilitate engineering tumor-targeted NPs, we have explored a simple and versatile method of modifying the NP surface. This method relies on the principle that dopamine is polymerized in a mild condition into an adhesive film (similar to mussel foot proteins), which can recruit nucleophilic functional groups. Using this method, the Yeo Lab has immobilized various surface modifiers (folate, RGD peptide, chitosan, and synthetic polymers) on polymeric NPs and observed that the modified NPs showed the intended interactions with target cells. A unique advantage of this method is that it is applicable to virtually any types of NPs including polymer, metal, and lipid-based NPs. This flexibility allows one to design core particles according to the applications, not constrained by the needs for surface modification. It also makes it easier to engineer functionally complex NPs, which would otherwise involve multiple inefficient steps. We take advantage of this versatility to investigate how surface chemistry of a NP dictates its biological fate in the body and determine design criteria for clinically effective NP drug carriers. Related publications
Intracellular delivery of peptide antibioticsIntracellular bacterial infections are significant medical problems, which can cause debilitating damages to the infected patients. Infections with these pathogens are currently managed by systemic administration of antibiotics. However, their therapeutic outcomes have been disappointing, because of the inefficient intracellular delivery of antibiotics and frequent emergence of bacterial resistance to the treatment. For effective management of intracellular bacterial infections, there is a critical unmet need for new types of antimicrobials, which will treat persistent and multi-drug resistant intracellular bacterial infections, and an appropriate carrier system that will deliver the new agents specifically to the infected macrophages and the pathogens resident in the cells. We aim to develop effective treatment of intracellular bacterial infections based on recent advances in peptide chemistry and drug delivery technology. Ideal treatment of intracellular pathogens should have low potential to induce bacterial resistance and be able to travel across the eukaryotic cell membrane and access pathogens residing inside the cells. To satisfy these requirements, We develop antimicrobial semi-nanoparticles (SNPs), consisting of ZWC and cationic antimicrobial peptides (CAMPs). The rationale of this approach is that CAMPs are less susceptible to bacterial resistance than traditional low molecular weight antibiotics, and a SNP form of CAMPs can take advantage of phagocytosis in entering macrophages and accessing the in vivo niche of intracellular pathogens. Moreover, the pH-sensitivity of SNP formulation will promote cytosolic CAMP release and their trafficking into intracellular target locations for effective killing of the pathogens. Related publications
Anion-resistant non-viral gene vectorsNon-viral vectors have been considered a promising alternative to viral vectors for the delivery of gene therapeutics. A critical limitation of non-viral vectors, which are mostly based on cationic lipids or polymers, is that their gene transfection efficiency diminishes greatly in the anionic environment prevalent in the body. The cellular toxicity of cationic polymers is another challenge that hampers in-vivo application of the non-viral vectors. We reported that a ternary gene-polymer complex consisting of hyaluronic acid, disulfide-crosslinked polyethyleneimine (PEI), and plasmid DNA was relatively non-toxic and achieved significantly higher transfection efficiency than other polymer systems, especially in the presence of serum. This welcome result is attributable to several features of the ternary system. First, the disulfide-crosslinked PEI degrades into smaller pieces in the cells, avoiding the toxic effect of high-molecular-weight PEI. Second, hyaluronic acid protects the gene-polymer complex in the extracellular environment and at the early stage of intracellular trafficking. Third, hyaluronic acid and disulfide-crosslinked PEI cooperate to facilitate a timely unpacking of DNA from the complex. Recently, the polymer components of the ternary complex have been further modified to achieve greater serum stability and greater target specificity. Related publications
Zwitterionic chitosan (ZWC) as a potential treatment of infectious diseasesAlthough ZWC was originally developed for NP surface modification, it was later recognized that ZWC was able to suppress the production of pro-inflammatory cytokines from endotoxin-challenged macrophages. We investigate the mechanism by which ZWC inactivates the endotoxin or the endotoxin-challenged macrophages and tries to take advantage of this unique property for the treatment of sepsis and extracorporeal purification of septic blood. Recently, we have discovered in collaboration with Dr. Chang Kim (Veterinary Medicine) that orally administered ZWC can also provide a local anti-inflammatory effect in the distal colon, protecting animals from chemical challenges that induce colitis. Related publications
Intraperitoneal drug delivery via in-situ crosslinkable hydrogelsHydrogels are attractive materials for a variety of biomedical applications due to their permeability, flexibility, biocompatibility, and structural similarity to the extracellular matrix. We have demonstrated that a hydrogel was an excellent delivery medium for prolonging the drug residence time and enhancing the pharmacological effect in the peritoneal cavity. Tissue-type plasminogen activator or budesonide delivered via a hyaluronic acid hydrogel to the injured peritoneum showed a dramatic anti-adhesion effect, far exceeding that of the free drug or the hydrogel alone. On the basis of this promise, we test whether the hydrogel can serve as a delivery medium for antiproliferative drugs in the therapy of intraperitoneal malignancies. We have demonstrated that the hydrogel could effectively retain paclitaxel in the pertioneal cavity and improved the local availability of the drug. Related publications
|